Research project launched under Charité management
Berlin, 16, January 2024
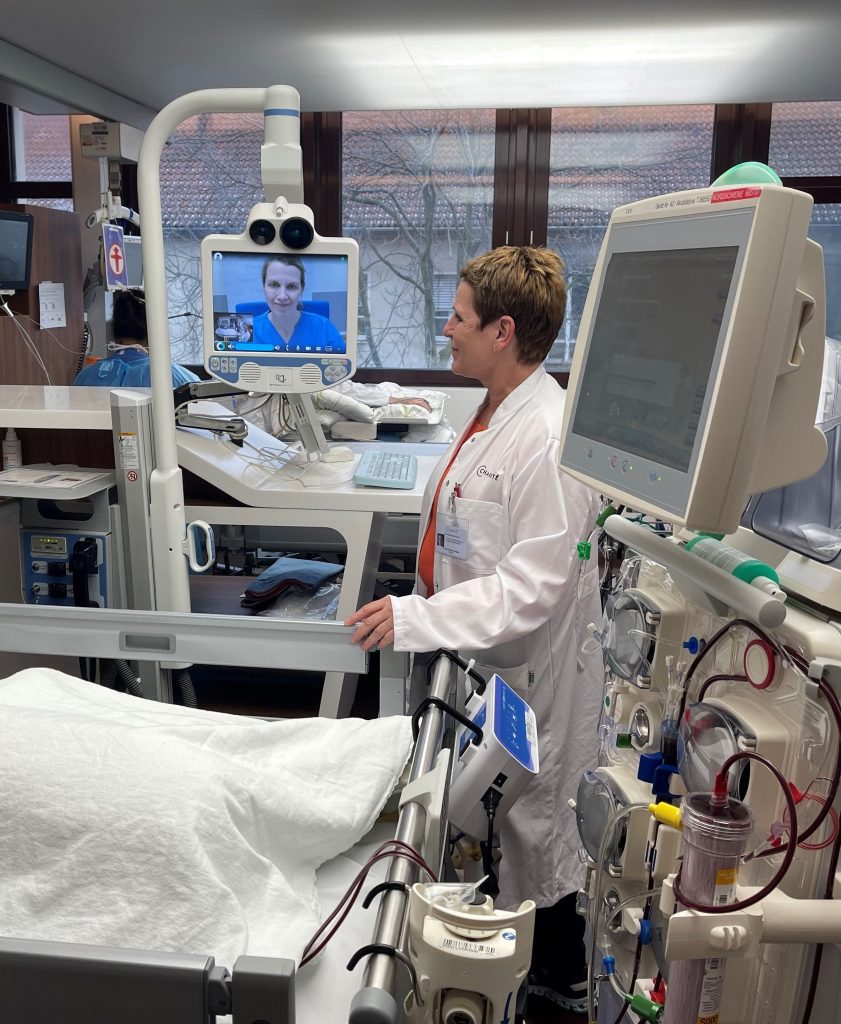
Palliative care for patients is standard practice in intensive care units. However, not every hospital has specialised palliative care expertise. Can telemedical consultations further improve palliative care in intensive care units? An international research consortium led by Charité – Universitätsmedizin Berlin is investigating this question. The project “Enhancing palliative care in ICU” (EPIC), which has now been launched, is being funded by the EU Commission for five years with around 6.3 million euros.
The goal of palliative medicine is to alleviate the suffering, pain and other symptoms of seriously ill patients in a targeted manner in order to preserve and promote their quality of life in the best possible way. It is an important and established part of intensive medical care. However, if the clinical picture and symptoms are very complex, it can be helpful for intensive care staff to seek advice from specialised palliative care physicians on the specific case. “However, not all hospitals have palliative care expertise in-house,” says Professor Claudia Spies, Director of the Department of Anaesthesiology and Intensive Care Medicine at Charité. “The systematic use of telemedicine, which allows experts to be consulted virtually and therefore quickly and from any location, could significantly improve palliative care in intensive care units.”
Triad of the practice model: further training, checklists, telemedicine
How great is the benefit of telemedical consultations by palliative care experts compared to conventional palliative care in intensive care units? This is what the research team is investigating as part of the EPIC project. “Before the telemedical counselling phase begins, the hospital staff in the intensive care units first receive palliative care training,” explains Claudia Spies, who is leading the research project. “We are also developing checklists to help the teams identify patients who would benefit from specialised palliative care as early as possible.” Around 2,000 patients and their family members are taking part in the research project. It is being carried out in seven clinical centres with palliative care and 23 multidisciplinary intensive care units in five European countries.
“With EPIC, we are bringing together clinicians and researchers from the fields of palliative and intensive care, social sciences, nursing sciences, ethics and health economics and want to implement a harmonised practice model for palliative care in intensive care units – across Europe,” says Claudia Spies. “We hope that our project will result in recommendations for action that we can make available to specialist organisations and that can be incorporated into the training and further education of the next generation of multiprofessional intensive care physicians.”
Shorter length of stay in the intensive care unit
Studies show that providing palliative care as early as possible shortens the time patients spend in intensive care, but does not affect mortality. With EPIC, the researchers are therefore also pursuing the goal of shortening the length of stay in intensive care units – which has health economic benefits, but is particularly invaluable for those affected. “Patients with serious, incurable illnesses who receive optimal palliative care will hopefully not spend their last days in intensive care – unless there is a serious reason. This can be a blessing for them and their families in this extremely critical and highly vulnerable phase at the end of life,” says Claudia Spies. “But even seriously or chronically ill people who are not at the end of their lives receive palliative care. Palliative care is not end-of-life care, which is a common misconception. Around half of patients can be discharged home to specialised palliative care. Improved palliative care across the board would therefore benefit all patients in intensive care units.”
With EPIC, the researchers also want to investigate how well palliative medical care with telemedical support is perceived and accepted by patients and their relatives. Furthermore, a patient and family group is to be established in which those affected can exchange information and support each other.
About EPIC
The research consortium is led by Prof Claudia Spies, Director of the Department of Anaesthesiology and Intensive Care Medicine at Campus Charité Mitte and Campus Virchow-Klinikum. Funding is provided by the European research framework programme “Horizon Europe”. Other partners in the consortium are: General University Hospital in Prague (Czech Republic), Hebrew University of Jerusalem (Israel), Heinrich Heine University Düsseldorf, King’s College Hospital (UK), KU Leuven (Belgium), Martin Luther University Halle-Wittenberg, Medical Faculty of the University of Basel (Switzerland), National and Kapodistrian University of Athens (Greece), Università degli Studi di Perugia (Italy), University of Southern Denmark (Denmark), Universitätsklinikum Erlangen, European Association for Palliative Care (Belgium), European Society of Anaesthesiology and Intensive Care (Belgium), tp21 GmbH. Cooperation with a patient and relatives’ organisation is planned.
Image: The team from the EU EPIC project aims to improve palliative care in intensive care units using telemedicine © Charité | Robert Gülland
