Charité study discovers brain network whose stimulation has a symptom-relieving effect
Berlin, 14 December 2022
Alzheimer’s disease is the most common cause of dementia, but so far it is not easily treatable. A possible future form of therapy could be so-called deep brain stimulation, also known as a brain pacemaker. In a study published in the journal Nature Communications*, a research team at Charité – Universitätsmedizin Berlin identified a specific network in the brains of Alzheimer’s patients whose stimulation was associated with symptom relief. The researchers hope the study will pave the way for further research.
Deep brain stimulation (THS) is a therapeutic procedure that is already approved in Germany for the treatment of neurological movement disorders such as Parkinson’s disease and dystonia, as well as for neuropsychiatric disorders such as obsessive-compulsive disorder. Ultra-fine electrodes are implanted in the brain of the patient, which continuously emit weak, short electrical impulses to the respective brain regions. The electrodes remain permanently in the brain and are connected to a pacemaker in the chest via cables that run under the skin. The current intensity and frequency can be adjusted via the pacemaker.
“Although THS has been established for the treatment of Parkinson’s for more than 20 years and the costs are covered by statutory health insurance, this form of therapy is still relatively unknown in general,” says Prof. Dr. Andreas Horn, head of a research group on network-based brain stimulation, which is based both at the Department of Neurology with Experimental Neurology at Charité Campus Mitte and at Brigham & Women’s Hospital and Massachusetts General Hospital within Harvard Medical School in Boston, USA. “THS works very well for Parkinson’s, and patients’ quality of life improves significantly.” Alzheimer’s, like Parkinson’s, is a neurodegenerative disease, so a potential therapeutic application of THS would be obvious. But for a safe and effective treatment, the target regions in the brain to be stimulated must be known very precisely.
The starting point for the current study, which was conducted in close collaboration with the University of Toronto, Canada, among other collaborating partners, was a chance observation in a Canadian study. “Deep brain stimulation triggered flashbacks – sudden memories from childhood and adolescence – in a patient who was being treated for obesity,” says Dr. Ana Sofía Ríos of the Department of Neurology with Experimental Neurology at Charité Campus Mitte and first author of the study. “So it was reasonable to assume that the stimulated brain region, which was located in the area known as the fornix, might also be suitable for treating Alzheimer’s disease.”
To investigate, researchers at seven international centers implanted electrodes in this area of the fornix in participants with mild Alzheimer’s disease as part of another multicenter study. “Unfortunately, most patients showed no improvement in Alzheimer’s symptoms. But a few study participants benefited significantly from the treatment,” Dr. Ríos says. “We wanted to find out how this difference occurred, and to do so we compared the exact position of the electrodes between the study participants.”
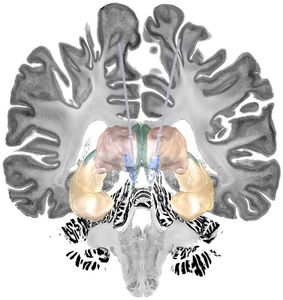
Prof. Horn’s research group specializes in analyzing high-resolution images of the brain taken using magnetic resonance imaging and, in combination with computer models, pinpointing the optimal stimulation points for THS in the brain with high precision. “One particular challenge here is that every brain is different. And that plays a big role in implanting the electrodes,” says Prof. Horn. “If you’re off by just a few millimeters, the expected effect may not occur.” That was also the case for the majority of the study participants. However, Prof. Horn’s research team was able to precisely determine the exact position of the electrodes in those Alzheimer’s patients in whom THS had an effect, based on the image data in the follow-up. “It is located at a branch point between two nerve fiber bundles – the fornix and the stria terminalis – which connect low-lying brain regions. Both structures are associated with memory function,” the neuroscientist explains.
Further clinical studies are needed before THS can be approved and used for the treatment of Alzheimer’s disease. The results of Prof. Horn’s research team provide an important basis for this. “If our data help to ensure that the electrodes can be placed more precisely in neurosurgical studies to test THS in Alzheimer’s, that would be great,” says Prof. Horn. “Because for Alzheimer’s, we urgently need an effective and symptom-relieving therapy to help patients – THS is a promising approach for this.”
In future research, Prof. Horn’s team will investigate and specify further networks of neurons in the brain that could be relevant for potential therapies for dementia. Among other things, the researchers will take a closer look at areas of brain damage and, in addition to targets for THS, include those for other neurostimulation procedures in their investigations.
*Ríos AS et al. Optimal Stimulation Sites and Networks for Deep Brain Stimulation of the Fornix in Alzheimer’s Disease. Nat Comm 2022 Dec 14. doi: 10.1038/s41467-022-34510-3
Caption: In people with Alzheimer’s disease, deep brain stimulation of the neuronal area between the fornix (green) and the stria terminalis nucleus area (blue) has shown the strongest beneficial effects. Additionally, the two brain structures thalamus (pink) and hippocampus (yellow) as well as the stimulation electrodes are shown. © Charité | Ana Sofía Ríos
Links:
Originalpublikation
Klinik für Neurologie mit Experimenteller Neurologie
Bewegungsstörungen gezielter behandeln (Pressemitteilung v. 01.04.2022)
Wie entstehen Tics? (Pressemitteilung v. 19.01.2022)
Nervenbahnen unter Strom (Pressemitteilung v. 03.07.2020)
Zwei neue Emmy Noether-Nachwuchsgruppen an der Charité (Pressemitteilung v. 20.03.2019)
