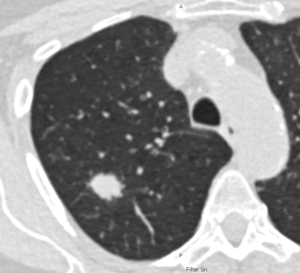
IMAGE: Lung CT © Charité | Jens Vogel Claussen
Berlin, November 14, 2025
To reduce the high mortality rate of lung cancer, a screening program is to be introduced in Germany. It is aimed at people aged 50 and over who have been heavy smokers for a long time. A publication by Charité – Universitätsmedizin Berlin, Hannover Medical School (MHH), the Grosshansdorf Lung Clinic, and the University Hospital Schleswig-Holstein (UKSH) now shows that if participants are selected not only based on their age and smoking history, but also according to additional criteria, more cases of cancer can be detected early. As the research team describes in the journal The Lancet Oncology*, this is particularly relevant for women.
Every year, around 57,000 people in Germany are diagnosed with lung cancer – often with fatal consequences because the disease is typically detected too late. A new screening program is expected to start in April 2026, which will use computed tomography (CT) scans to check for suspicious changes in the lungs of people at high risk of developing lung cancer. Currently, lung cancer screening is planned to be offered to individuals between 50 and 75 years of age who – to put it simply – have been heavy smokers for over 25 years.**
“Our data show that, based on these criteria, we are overlooking some people who also have a high risk of lung cancer and would benefit from the early detection program,” says Prof. Jens Vogel-Claussen, head of the now-published HANSE study. “If we consider more factors than just age and smoking history, we detect almost 20 percent more cases of lung cancer,” the radiologist emphasizes. Since October, he has been Director of the Department of Radiology at Charité. He previously initiated the HANSE study at Hannover Medical School (MHH) and continues to oversee it there as principal investigator.
The study, conducted within the framework of the German Center for Lung Research (DZL), investigated how well CT screening detects lung cancer at an early stage when participants are selected according to a comprehensive set of criteria, the so-called PLCOm2012 score. In addition to age and smoking history, it also considers a person’s level of education, weight, the presence of chronic obstructive pulmonary disease (COPD), previous cancer diagnoses, and whether there is a family history of lung cancer.
The results were compared with the selection criteria intended to underlie the planned lung cancer screening program, which considers only age and smoking history (the “Nelson score”). All individuals identified as having a high risk of lung cancer based on either score underwent two low-dose CT scans, one year apart, as part of the study. Suspected cases were reviewed in interdisciplinary case conferences, and treatment was initiated if confirmed.
Among approximately 4,200 current or former smokers screened using the PLCOm2012 score, researchers found 108 cases of lung cancer. This is 19.4 percent more than in the NELSON control group of approximately 3,900 people, where 85 cases of cancer were detected. “If we use the more comprehensive PLCOm2012 score with a defined threshold, we have to screen about 6 percent more people, but we find significantly more cases of lung cancer,” explains Prof. Martin Reck, Head of the Oncology Department at the Grosshansdorf Lung Clinic and senior author of the study. “This makes screening more efficient; we need to perform fewer CT scans to diagnose a case of lung cancer.”
Women, in particular, benefit from the expanded set of criteria. On the one hand, they are disproportionately affected: In the HANSE study, a total of 2.6 percent of women received a lung cancer diagnosis, compared to 1.8 percent of men. On the other hand, they more frequently fall outside the scope of the narrowly defined criteria. “Many of the women in our study are active smokers, but have smoked fewer cigarettes over their lifetime than the men and therefore do not meet the current inclusion threshold in Germany,” explains Dr. Sabine Bohnet, head of the Lung Cancer Center at the Lübeck campus of the University Hospital Schleswig-Holstein (UKSH) and co-author of the study. “Furthermore, they are more likely to have, for example, a family history of lung cancer, their own history of cancer, or an additional COPD diagnosis. We assume that these risk factors have a greater impact on women than on men. Unfortunately, they are not addressed by the currently applicable criteria.”
The planned early detection screening aims to reduce mortality from lung cancer by detecting and treating the disease early. “Our study has shown that it is both possible and necessary to change the inclusion criteria for screening based on the results of the HANSE study,” summarizes Jens Vogel-Claussen. “Otherwise, we will overlook important risk groups.”
*Vogel-Claussen J et al. Effectiveness of NELSON versus PLCOm2012 lung cancer screening eligibility criteria in Germany (HANSE): a prospective cohort study. Lancet Oncol 2025 Nov 10. doi: 10.1016/S1470-2045(25)00490-5
**According to current plans, those eligible for lung cancer screening are: individuals with statutory health insurance between the ages of 50 and 75 who have smoked for at least 25 years and either still smoke actively or quit less than ten years ago. The amount of tobacco consumption must be calculated to be at least 15 pack-years (one pack-year is 20 cigarettes per day for one year).
About the HANSE Study
The HANSE study is an investigator-initiated trial, meaning it was initiated by the researchers themselves. The NELSON inclusion criteria were compared with a PLCOm2012 score, which corresponds to a six-year risk of developing lung cancer of at least 1.58 percent. Participants were recruited at Hannover Medical School (MHH), the University Hospital Schleswig-Holstein at the Lübeck Campus, and the Grosshansdorf Lung Clinic. All three locations are certified lung cancer centers by the German Cancer Society (DKG). The study was funded by the German Center for Lung Cancer (DZL) and, within the framework of the Lung Ambition Alliance, by AstraZeneca. The HANSE study will continue: Between autumn 2025 and summer 2026, participants already enrolled who have a high risk of lung cancer will receive another CT screening. Furthermore, the study will investigate for the first time whether biomarkers in the blood can be identified that could enable even earlier diagnosis of lung cancer in the future. The aim is to further improve the precision and effectiveness of the screening.
Image: Low-dose CT scan of the lungs of a 69-year-old female smoker. The white, rounded area in the lung tissue indicates early-stage lung cancer. At this stage, lung cancer is still highly treatable. © Charité | Jens Vogel-Claussen
SOURCE: Joint press release from Charité, MHH, UKSH and LungenClinic Grosshansdorf

Leave a Reply