How a well-known compound can become a game-changer
Berlin, 13.04.2022
More and more drugs are available for the treatment of COVID-19. Researchers at Charité – Universitätsmedizin Berlin, the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) and Freie Universität (FU) Berlin have studied the mechanisms of action of antiviral and anti-inflammatory substances in more detail. In the scientific journal Molecular Therapy*, they describe that a combination of both works best and extends the time window for the use of antibody therapy.
Infections with SARS-CoV-2 still also lead to hospital admissions. Currently, according to the Robert Koch Institute, about six to seven people with COVID-19 are admitted within one week per 100,000 inhabitants. In the inpatient treatment of COVID-19 patients, there are now a number of drugs that mitigate the course of the disease or reduce the risk of a fatal outcome in severely ill patients. Some fight the virus, others the inflammation it causes.
In particular, monoclonal antibodies and the powerful anti-inflammatory drug dexamethasone are used. Antibodies intercept the virus and attach to the surface of the spike protein, preventing it from entering human cells. This therapy is used until the seventh day after the onset of symptoms. Oxygen-dependent COVID-19 patients in hospital are usually given dexamethasone. This glucocorticoid has been used for about 60 years to treat some inflammatory conditions caused by excessive activation of the immune system. It also reliably dampens the body’s inflammatory reaction in COVID-19. However, the active ingredient is associated with various side effects; for example, it can cause fungal infections. Therefore, the remedy should only be used in a very targeted manner.
Scientists from the Charité, the Berlin Institute for Medical Systems Biology (BIMSB) at the MDC and the FU Berlin have investigated the mechanisms of action of both therapies. “We found evidence that a combination of antibody and dexamethasone therapy works better than the individual therapies on their own,” says Dr. Emanuel Wyler, scientist in the RNA Biology and Posttranscriptional Regulation research group headed by Prof. Dr. Markus Landthaler at the BIMSB, and first author of the study.
Since not all lung areas can be examined using samples from patients, the research teams first looked for a suitable model last year. Co-last author Dr. Jakob Trimpert, veterinarian and working group leader at the Institute of Virology at the Free University of Berlin, developed COVID-19 hamster models in this course. Animals are currently the most important non-transgenic model organism for COVID-19, as they are infected with the same viral variants as humans and develop similar disease symptoms. The disease progresses differently in the individual species: golden hamsters only contract the disease moderately, while Roborovski dwarf hamsters show a severe course similar to that of COVID-19 patients in intensive care units.
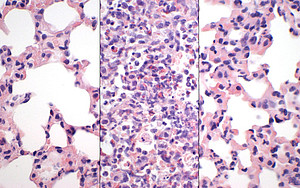
“In the current study, we tested the effects of separate and combined antiviral and anti-inflammatory treatments for COVID-19, i.e. with monoclonal antibodies, dexamethasone or a combination of both therapies, in the existing models,” explains Dr Trimpert. To analyse the extent of the damage to the lung tissue, the veterinary pathologists at the FU Berlin examined infected lung tissue under the microscope. In addition, Dr Trimpert’s team determined the amount of infectious viruses and viral RNA at different times during the treatment. This enabled the researchers to check whether and how the viral activity changed during the course of the therapy. “With the help of detailed analyses of various parameters of a COVID-19 disease, which are only possible in this way in the animal model, we have not only succeeded in better understanding the basics of the mode of action of two particularly important COVID-19 drugs, we also found clear indications of possible advantages of a combination therapy of monoclonal antibodies and dexamethasone,” says Dr Trimpert.
Single cell analyses have shown the influence of the drugs on the complex interplay of signalling pathways within the tissue cells and on the number of immune cells. The researchers run the individual cells of a sample over a chip. There they are packed into small aqueous droplets together with a barcode. In this way, the RNA – the part of the genetic material that the cell had just read – can be sequenced and later reassigned to the cell. From the data obtained, the function of the cell can be deduced with high precision. “We were able to observe, for example, that the antibodies were able to efficiently reduce the amount of virus,” explains Dr Wyler. “However, this did not help much in the model.” This is because it is not the viruses that damage the lung tissue, but the strong inflammatory reaction they trigger. The immune cells that fight the invaders release messenger substances to call for reinforcement. The masses of defence fighters that flood in can literally clog up the lungs. “Blocked blood vessels and unstable vascular walls can then lead to acute lung failure,” the scientist explains.
The well-known dexamethasone caused a surprise. “The anti-inflammatory has a particularly strong effect on a specific type of immune cell, the neutrophils,” says co-lead author Dr. Geraldine Nouailles, scientific working group leader at the Charité Medical Clinic with a focus on infectiology and pneumology. The neutrophils belong to the white blood cells and come on the scene very quickly during infections with viruses and bacteria. “The cortisone preparation suppresses the immune system and prevents the neutrophils from producing messenger substances that attract other immune cells,” Dr Nouailles explains. “In this way, the drug is very effective in preventing an escalation of the immune response.”
The researchers achieved the best treatment results when they combined the antiviral with the anti-inflammatory therapy. “So far, medical guidelines do not provide for such a combination therapy,” Dr Nouailles emphasises. “In addition, antibody therapy may so far only be administered up to a maximum of the seventh day after symptom onset in high-risk patients. In practice, dexamethasone is only administered when patients become oxygen dependent, i.e. their disease is already far advanced. The combination, on the other hand, opens up a whole new window of treatment.” An approach that now has to be tested in clinical trials before it can be considered for the treatment of patients.
*Emanuel Wyler et al. Key benefits of dexamethasone and antibody treatment in COVID-19 hamster models revealed by single cell transcriptomics. Molecular Therapy (2022). doi: https://doi.org/10.1016/j.ymthe.2022.03.014
About the study
The work was funded, among others, by the German Research Foundation (DFG) in the Collaborative Research Centre SFB-TR84, the Federal Ministry of Education and Research (BMBF) with the CAPSyS-COVID and PROVID projects and the Berlin Institute of Health (BIH) at the Charité with CM-COVID. The study was also made possible by the BMBF-funded National Research Network of University Medicine on Covid-19 (NUM), in the Organostrat sub-project.
Links:
Originalpublikation
Fachbereich Veterinärmedizin der FU Berlin
BIMSB AG Landthaler
Pressemitteilung zu vorangegangener Publikation 08/2021 in Nature Communications
